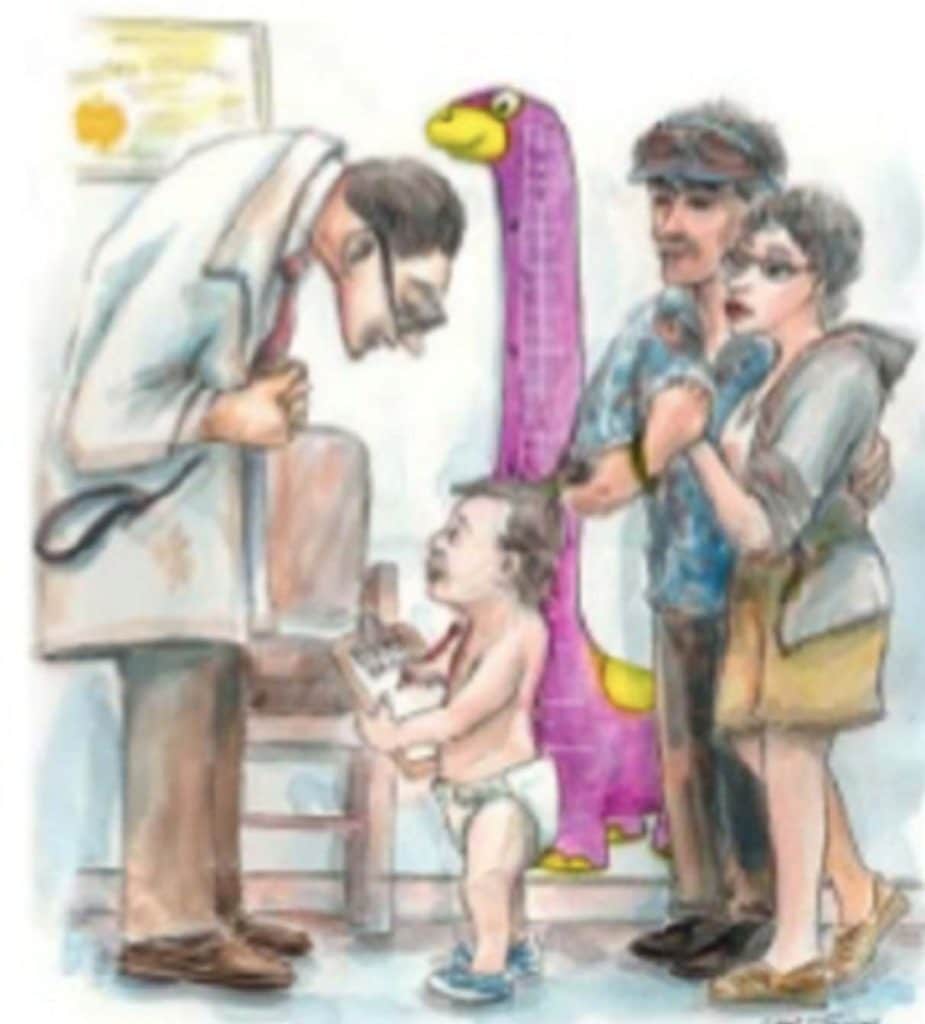
Growth charts have been used for at least a century to assess whether a child is receiving adequate nutrition and to screen for potentially inadequate growth that might be indicative of adverse health conditions.
Pediatric Stages of Development:
| Stage | Description |
|---|---|
| Preterm | Birth < 37 weeks’ gestation |
| Neonate | Newborn to 1 month |
| Infant | 1 month 12 months |
| Toddler | 12 months to 36 months |
| Child | 3 years to 12 years |
| Adolescent | 12 years to 18 years |
The physical growth of infants and children has long been recognized as an important indicator of health and wellness.
Why Is It Important to Assess Growth and Nutrition During the Physical Examination?
People can have an optimal nutritional status or they can be under-, over- and/or malnourished.
Traditionally, attention has focused on under-nutrition. However, in the past few decades, concerns about excessive weight gain have increased, and growth charts have been used to screen for overweight, including obesity.


Factors that Affect Child Growth:
Hormones Regulating Growth:
- Growth hormone.
- Thyroid hormones:
- Growth is severely stunted in hypothyroid children.
- Hypersecretion does not cause excessive growth.
- Insulin & IGF 1:
- Deficiency often blocks growth.
- Hyperinsulinism often spurts excessive growth.
- Androgens:
- Play a role in pubertal growth spurt, stimulate protein synthesis in many organs.
- Effects depend on presence of GH.
- Perinatal period
- Maturation of the CNS is absolutely dependent on thyroid hormone
- Thyroid hormone deficiency causes irreversible mental retardation
- Adulthood:
- Hyperthyroidism causes hyperexcitability and irritability
- Hypothyroidism causes decrease mental capacity & impaired memory
Postnatal Growth:
- Growth hormone, insulin, and thyroid hormone play major roles.
- Replacement of hormone deficiencies creates a period of catch-up growth, but it is soon replaced with a normal growth rate.
- There is no major role for gonadal sex steroids or for glucocorticoids on prepubertal growth but glucocorticoid excess will slow child growth.

Heredity and Environment play important roles in a child’s growth and development:
- Heredity or “nature”.
- Strong influence on physical development.
- Includes the physical make up the child inherits from parents.
- Environment or “nurture”.
- Everything that surrounds and influences a child.
Measurement Parameters:
- Linear growth (Length/Height).
- Weight and body mass index.
- Weight/Height.
- Head circumference; HC/CC ratio.
- Mid arm circumference.
- Body proportions (arm span and upper-to-lower segment ratio).
- Growth velocity.
- Growth patterns.
- Dentition.
- Bone Age.
Postnatal growth patterns of normal children are well characterized, resulting in several clinical parameters for assessment of child growth.
| Linear growth |
|---|
| length |
| height |
| length in normal infant |
| half adult height |
| height at 5 years |
| HEIGHT VELOCITY: (MORE SENSITIVE MEASURE) |
|---|
| birth and 6 months |
| 7 to 12 months |
| 12 months and 10 years |
| Factors affecting height velocity |
|---|
| Before 12 months |
| After 12 months |
Length is measured in children too young to stand; height is measured once the child can stand.
Height:
Full l-term infants increases about 30% by 5 months and > 50% by 12 months; infants grow about 25 cm during the first year.
In most boys, half the adult height is attained by about age 2; in most girls, height at 19 months is about half the adult height. Height at 5 years is about double the birth length.
Formulas for Calculating Midparental Height in Children:
Girls:
[Paternal height (cm) — 13 cm + maternal height (cm)] / 2
Or
[Paternal height (in) — 5 in + maternal height (in)] / 2
Boys:
[Paternal height (cm) + 13 cm + maternal height (cm)] / 2
Or
[Paternal height (in) + 5 in + maternal height (in)] / 2
Height is a more sensitive measure of child growth than time-specific height measures. In general, healthy term infants and children grow about 2.5 cm/month between birth and 6 months, 1.3 cm/month from 7 to 12 months, and about 7.6 cm/year between 12 months and 10 years.
Height varies and is due in part to perinatal factors (eg, prematurity). After 12 months, height is mostly genetically determined, and height velocity stays nearly constant until puberty; a child’s height relative to peers tends to remain the same.
Weight:
| Normal term neonates |
|---|
| 0 – 3 months |
| 3- 12 months |
| 2x birth weight |
| 3xbirth weight |
| 4x birth weight |
| 2 years to puberty |
| Head circumference (Reflects brain size measured up to 36 months) |
|---|
| At birth |
| During the first year |
| 2 years |
| 3 years |
| 7 years |
- Head circumference increases an average 1 cm/month during the first year; child growth is more rapid in the first 8 months, and by 12 months, the brain has completed half its postnatal growth and is 75% of adult size.
- Head circumference increases 3.5 cm over the next 2 years; the brain is 80% of adult size by age 3 years and 90% by age 7 years.
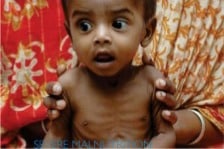
Measuring fat-free mass (muscle mass):
An accurate way to measure fat-free mass is to measure the Mid Upper Arm Circumference (MUAC). What is the MUAC?
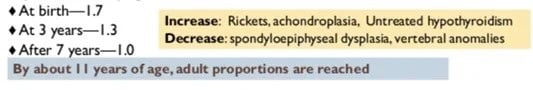
Upper-to-Lower Segment Ratio:
The upper-to-lower segment ratio is calculated when a child’s body may have inappropriate proportions between the head and trunk to the extremities.
Measure the lower body segment (distance from the symphysis pubis to the floor when a child stands).
Calculate the upper body segment by subtracting the lower body segment from the total height. Then divide the upper body segment by the lower body segment to calculate the ratio.
Expected ratios by age are:
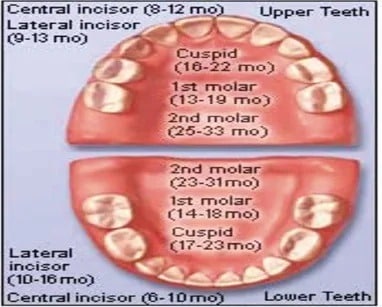
Primary Teeth Development Chart:
| Upper Teeth | When tooth emerges | When tooth falls out |
|---|---|---|
| Central incisor | 8 to 12 months | 6 to 7 years |
| Lateral incisor | 9 to 13 months | 7 to 8 years |
| Canine (cuspid) | 16 to 22 months | 10 to 12 years |
| First molar | 13 to 19 months | 9 to 11 years |
| Second molar | 25 to 33 months | 10 to 12 years |
| Lower Teeth | When tooth emerges | When tooth falls out |
|---|---|---|
| Second molar | 23 to 31 months | 10 to 12 years |
| First molar | 14 to 18 months | 9 to 11 years |
| Canine (cuspid) | 17 to 23 months | 9 to 12 years |
| Lateral incisor | 10 to 16 months | 7 to 8 years |
| Central incisor | 6 to 10 months | 6 to 7 years |
Primary Teeth Eruption Chart:
Bone Age:
The two most widely used systems are:
- The Greulich-Pyle Atlas method (GP method) in which a left-hand wrist radiograph is compared by means of a sequence of radiographs grouped in the atlas according to age and gender.
- The Tanner-Whitehouse 2 Bones method (TW2 method).
In which a maturity score is awarded to individual epiphyses, the sum of which is then converted to a bone age which is plotted on the growth chart as height for bone age.
How Should You Take These Measurements?
Measure Weight:
- Weigh younger infants nude or in a clean diaper on a calibrated beam or electronic scale. Weigh older infants in a clean, disposable diaper.
- Position the infant in the center of the scale tray.
- It is desirable for 2 people to be involved when weighing an infant. One measurer weighs the infant and protects him or her from harm (such as falling) and reads the weight as it is obtained. The other measurer immediately notes the measurement in the infant’s chart.
- Weigh the infant to the nearest 0.01 kg or 1/2 oz.
- Record the weight as soon as it is completed.
- Then reposition the infant and repeat the weight measurement. Note the second measurement in writing. Compare the weights. They should agree within 0.1 kg or 1/4 Ib. If the difference exceeds this, reweigh the infant a third time. Record the average of the 2 closest weights.
Calculate BMI:
- Choose English or metric calculation for BMI.
- English: (Weight (Ib) / [Stature (in) x Stature (in)]) x 703
- Metric: Weight (ka) / [Stature (m) x Stature (m)]
Measure Head Circumference:
Obtain an accurate head circumference, or occipital frontal circumference, by using a flexible non-stretchable measuring tape. Head circumference is generally measured on infants and children until the age of 3 years.
| HC > CC | Birth by 3 cm |
| HC = CC | 9 – 12 months |
| HC < CC | After 1 years |

