Muscular Dystrophy and Muscle Diseases
Muscular Dystrophy and Muscle Diseases
Helping Families Manage Progressive Muscle Weakness With Care and Clarity

At KidsHeart Medical Center, we support children facing muscle disorders — from initial symptoms to long-term care planning.
Muscular Dystrophies and related muscle diseases affect strength, mobility, and daily life.
Some conditions are inherited, others appear without warning. While these are often progressive, early diagnosis, therapy, and coordinated care can significantly improve outcomes.
Our Pediatric Neurology team provides expert guidance and ongoing support across Abu Dhabi, Dubai, and Al Ain.

What Are Muscular Dystrophies and Muscle Diseases?
Muscle diseases in children include a range of genetic and acquired conditions that cause weakness, fatigue, or delayed motor skills.
These may include:
- Duchenne Muscular Dystrophy (DMD)
- Becker Muscular Dystrophy
- Congenital Myopathies
- Inflammatory Muscle Disorders (e.g., juvenile dermatomyositis)
- Metabolic and mitochondrial muscle disorders
Common signs include:
- Trouble walking, running, or climbing stairs
- Frequent falls or toe-walking
- Enlarged calves or poor endurance
- Delayed motor milestones
- Progressive loss of strength over time
Many of these disorders require specialized genetic, neurological, and therapy input.
When Should You Seek Help?
See a Pediatric Neurologist if your child:
- Shows unexplained weakness or clumsiness
- Is losing motor skills they once had
- Tires easily or avoids physical activity
- Has a known family history of muscle disorders
- Was diagnosed with elevated creatine kinase (CK) levels
- Needs evaluation for a previously identified neuromuscular condition
The earlier we identify the cause, the better we can plan meaningful interventions.
How We Evaluate and Support Muscle Disorders
Here’s how we work with families facing muscle disease concerns:
- Clinical History and Family Background: We ask about symptoms, timing, and any family pattern of similar issues.
- Physical and Neuromuscular Examination: This helps us localize the weakness and determine what systems are affected.
- Blood and Genetic Testing: Tests may include creatine kinase (CK), DNA panels, or enzyme studies.
- EMG or Nerve Studies: In some cases, we assess how muscles and nerves communicate.
- Diagnosis, Therapy Planning, and Follow-Up: Based on the type of disorder, we involve physiotherapy, genetics, and sometimes cardiology or pulmonology.
We provide a long-term care roadmap — practical, supportive, and grounded in real-world needs.
Why Families Trust KidsHeart
- Pediatric Neurology specialists with neuromuscular expertise
- On-site diagnostics, including CK testing and EMG coordination
- Team-based approach involving rehab, cardiology, and pulmonology
- Emotional support and advocacy for families navigating complex diagnoses
- Centers in Abu Dhabi, Dubai, and Al Ain
We understand both the science and the day-to-day life behind these conditions — and we stand with you through both.

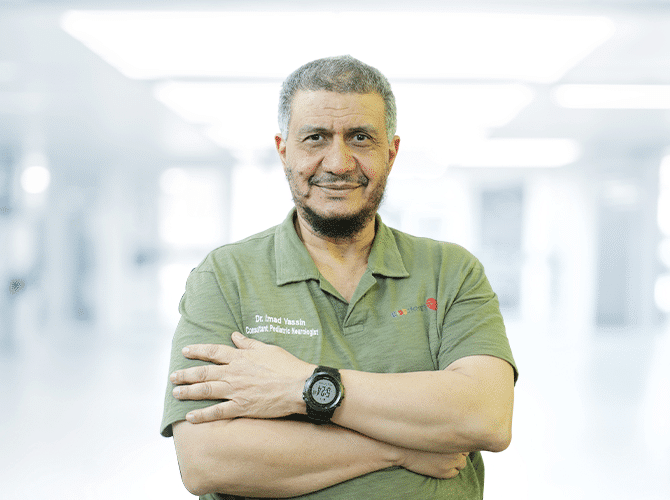
Dr. Imad Yassin
Consultant Pediatrician/ Pediatric Neurologist – FRCPCH(UK) | Facharzt, FAMAP, Pediatric Neurology Cert (Austria)
Seeing Muscle Weakness in Your Child? Let’s Find the Right Path Forward.
If you’re noticing motor concerns — or managing a known muscle condition — we’re ready to help.
Frequently Asked Questions (FAQs)
Not yet. But treatments are improving, and early care can delay progression and support quality of life.
Usually through clinical signs, blood tests (CK), genetic testing, and sometimes muscle biopsy or EMG.
It depends on the specific diagnosis and progression. We plan proactively, but not all children require one.
Most cause weakness, not pain — though some children develop joint or muscle discomfort as symptoms evolve.
We adjust based on the condition — typically every 3–6 months for active management and monitoring.

